The patient, a 70-year-old man with a shock of silver hair, is being treated in Yale New Haven Hospital’s neurocritical care unit (neuro ICU). You wouldn’t know from looking at him that his pituitary gland’s tumor had been removed a few days before. While the physicians entered his nose to get the tumor, as is customary, the procedure left no visible scars. He engages in animated conversation with two research colleagues who have come to monitor his progress with a novel and potentially ground-breaking technology they are testing.
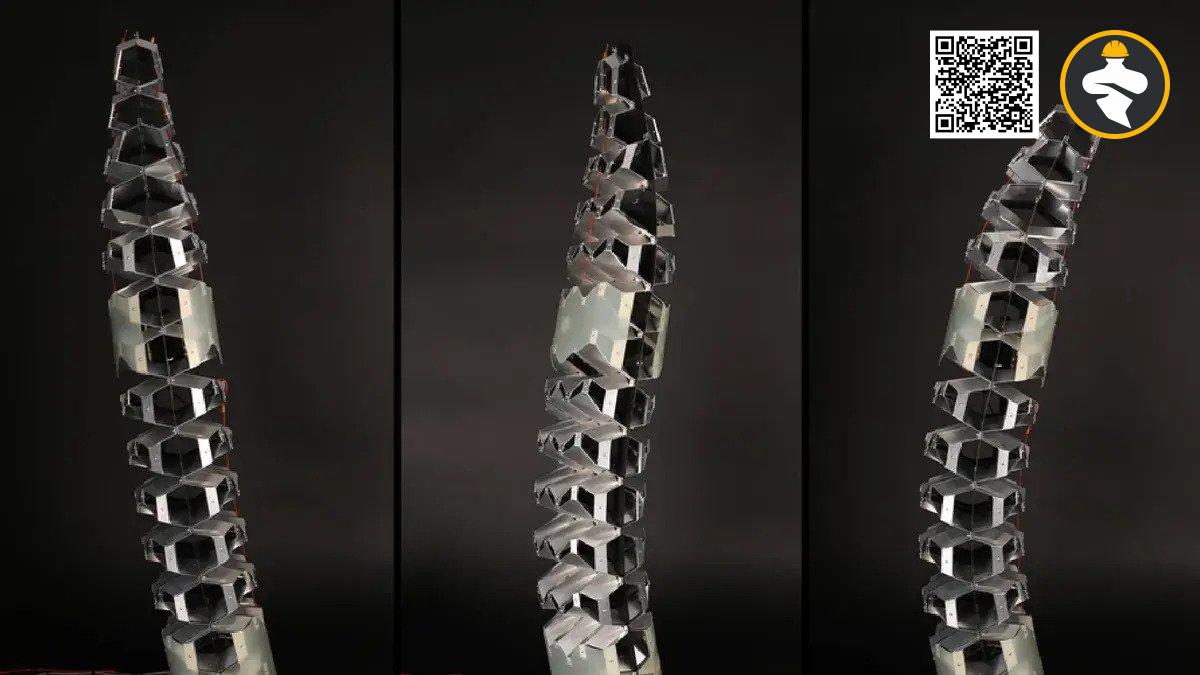
The tall, cylindrical gadget resembles R2D2 from Star Wars and might be his brooding older brother.
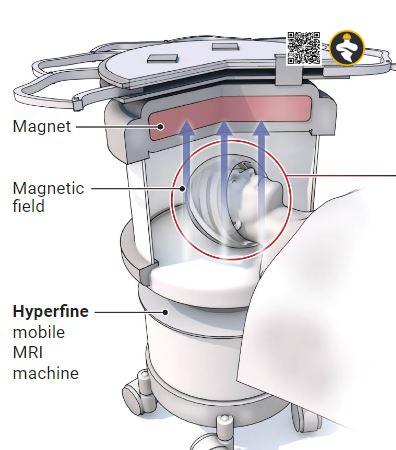
The 630-kilogram self-propelled scanner is cautiously steered up to the head of the bed by one of the researchers using a joystick. The researchers lift the man by his bed sheet and assist him in putting his head inside the Swoop, a mobile magnetic resonance imaging (MRI) scanner produced by the company Hyperfine.
The second researcher, Vineetha Yadlapalli, inquires, “Do you want earplugs?
Is the MRI louder than a typical MRI?
“Definitely not.”
“I suppose I don’t need them then.”
Yadlapalli positions the patient’s legs up to relieve pressure on his back before starting the machine by putting in a few commands from an iPad. The device begins to growl softly before beeping and clicking. Within minutes, Yadlapalli’s tablet displays a picture of the patient’s brain.
The man remains still for 30 minutes with his hands folded across his stomach. He might be setting his hair in a vintage hair dryer. He is a pioneer in a tiny manner, helping to advance MRI in uncharted territory.
Several scientists have been working on developing scanners for years that employ considerably smaller permanent magnets manufactured of the alloy frequently used in office toys. These create fields that are about 1/25th as powerful as a typical MRI magnet, which in the past would have been much too weak to provide a useful image. Nonetheless, several organizations have photographed the brain in such low fields—albeit with lesser resolution than typical MRI—thanks to improved electronics, more effective data gathering, and innovative signal processing techniques. As a result, scanners that can roll up to a patient’s bed and may be affordable enough to make MRI available everywhere are created.
Physicians are putting the Swoop through clinical testing at Yale New Haven and elsewhere after it received FDA permission in August 2020 to be the first low-field scanner to assess the brain. Other gadgets follow closely behind. However, due to the poorer resolution of a low-field scanner, Andrew McDowell, a physicist and the founder of the consulting company NeuvoMR, LLC, advises caution. Convincing doctors to begin utilizing it will be the true challenge, he claims. “That’s incredibly challenging because they’re quite conservative for legitimate reasons.”
All of this is made simpler by a greater field, which more fully polarizes the protons and generates a stronger signal. One tesla, or 30,000 times Earth’s magnetic field, is produced by a typical scanner’s magnet, while some scanners can create three or seven Tesla. Yet, only 0.001% more protons are pointed along a 1.5-tesla field than are pointed in the other direction. The polarization decreases by a factor of 25 with a reduction in field strength. Even more, by almost a factor of 300, the signal-to-noise ratio declines.
As radio astronomers separate a weak signal from noise by focusing their dishes on a star for hours or days, a low-field scanner might theoretically extract a signal from the noise by collecting data over a longer time period.
A human can only remain stationary for so long, thus that strategy won’t work with them. Hence, in order to create low-field MRI, scientists had to figure out how to extract data considerably more quickly.
Better hardware is a crucial component, according to Joshua Harper, a brain engineer at the German Paraguayan University. We now have extremely quick and affordable electronics, he claims. That’s truly the reason it works. Yet, performing low-field MRI in a hospital room is challenging. Static from other devices can interfere with the radio signal, and metal in other machinery or even the walls can distort the field. Scanners, therefore, use defense mechanisms. For instance, the Swoop product from Hyperfine employs antennae to detect radio noise and suppress it, just like noise-canceling headphones do.
In order to operate more quickly, the new scanners take advantage of a feature of the lower field. A high-field scanner can only pulse so quickly before it starts to heat the patient since it needs to employ higher frequency, higher intensity radio waves to manipulate the protons. According to Massachusetts General Hospital scientist Matthew Rosen, who also co-founded Hyperfine, a low-field scanner may pulse quicker and use more effective pulse sequences when it is not constrained by that speed constraint. We can question someone really quickly and in ways that you could never do in a high field.
Even yet, it is still difficult to collect data quickly enough for typical image reconstruction. Using cutting-edge signal processing methods, such as artificial intelligence, is one approach. According to Khan Siddiqui, chief medical officer and chief strategy officer at Hyperfine, engineers utilize a set of training photos to educate a program called a neural network to create brain images from relatively sparse data. “Where our secret sauce comes in is at that point.”
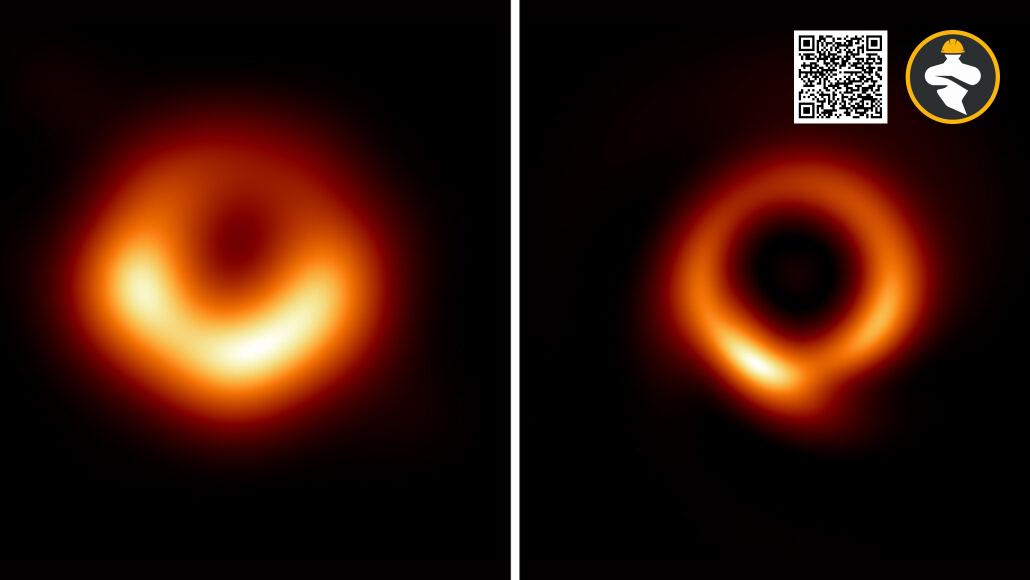
A low-field image appears blurrier when compared to a typical scan. Yet physicists appreciate its beauty. It’s this amazing physics success story, says Rosen. It’s not just us scientists with pointy heads “goofing off” and doing things that no one cares about. According to McDowell, the technology vindicates individuals toiling in a remote area of the field.
Who in their right mind would construct a 65 millitesla machine when constructing an 11 tesla one would bring them glory?
According to HYPERFINE, its SWOOP SCANner is off to a fairly fantastic start. More than 100 of the machines have been sold, the most of them in the United States, for about $250,000. The objective, according to Siddiqui, is to increase the usage of MRI rather than to replace high-field scanners. “Our mobile scanner reduces the distance and time between the MRI and the patient.” To quickly evaluate patients who are too unwell or unstable to be wheeled to a traditional MRI or a CT machine, which generates a form of 3D x-ray, Hyperfine anticipates deploying it in the neuro ICU.
Two disks make up a Swoop’s magnet, which generates a 64 millitesla field. A scan from it feels very dissimilar from a typical scan. A robotic table slides your body inside the cylindrical magnet of a traditional scanning. An adept patient can scooch into the magnet with the Swoop as though wriggling under a car’s bumper. Your head is cradled so tightly that it might touch your nose by a helmet-like head gear that houses the antennas, but your arms and legs are free. The chirping of the machine is gentle, almost calming.
Patients may be able to receive follow-up scans more frequently thanks to the less expensive, smaller devices. Ronald Walsworth, a physicist at the University of Maryland, College Park, and the co-founder of Hyperfine, finds that idea appealing. His kid, who was two years old at the time, suffered a benign brain tumor in 2007. According to Walsworth, a member of the advisory board for Hyperfine, he was effectively treated. “There were indicators that were not noticed early and things that were not decided most efficiently,” he claims, “since the MRIs could only happen seldom.”
It will soon be used in a project to examine the usefulness of low-field MRI in impoverished countries. An international nonprofit organization manages the 55-bed pediatric neurosurgery facility CURE Children’s Hospital of Uganda in Mbale, wants to contrast the CT scanner, a Quadcopter, and Obugoloch’s scanning. Children with hydrocephalus, in which cerebrospinal fluid accumulates in the brain and compresses it, may suffer fatal or disabling damage, are imaged by doctors. Every year, 400,000 children worldwide are diagnosed with hydrocephalus, which accounts for 75% of the patients at the CURE hospital. An infection is typically the cause in Africa.
Reference: Adrian Cho@science.org